Note: This blog post article is the third in a series of twelve articles on musculoskeletal conditions of the low back (lumbar spine) and pelvis. For the rest of the articles in the series, scroll to the end of this article.
Lumbar Spine Joint Dysfunction (Subluxation/Misalignment)
 Like hypertonic musculature, joint dysfunction is usually present as a component of most pathologic musculoskeletal conditions of the low back and pelvis. Tight muscles and joint dysfunction seem to follow a cyclical pattern. If tight muscles are present, they restrict joint motion, which leads to adhesions in the periarticular soft tissues (tissues located around the joint) and causes joint dysfunction. Similarly, if joint dysfunction is present, the lack of proper movement will either lead to adaptive shortening and tightening of the muscles, and/or the pain with attempted motion will cause splinting of the adjacent musculature. For this reason, most musculoskeletal problems involve a combination of tight musculature and joint dysfunction. The benefits of massage for the musculature are clear, as are the benefits of stretching for the musculature and joints and of joint mobilization for the joints.
Like hypertonic musculature, joint dysfunction is usually present as a component of most pathologic musculoskeletal conditions of the low back and pelvis. Tight muscles and joint dysfunction seem to follow a cyclical pattern. If tight muscles are present, they restrict joint motion, which leads to adhesions in the periarticular soft tissues (tissues located around the joint) and causes joint dysfunction. Similarly, if joint dysfunction is present, the lack of proper movement will either lead to adaptive shortening and tightening of the muscles, and/or the pain with attempted motion will cause splinting of the adjacent musculature. For this reason, most musculoskeletal problems involve a combination of tight musculature and joint dysfunction. The benefits of massage for the musculature are clear, as are the benefits of stretching for the musculature and joints and of joint mobilization for the joints.
Note: Massage and Chiropractic
Tight musculature and joint dysfunction usually coexist in every musculoskeletal condition. For this reason, massage therapy and chiropractic (or osteopathy) ideally complement each other, and massage therapists are often employed in chiropractic offices. In chronic conditions, fibrous adhesions are also nearly always present, reinforcing the need for chiropractic manipulation and massage as well as moist heat and stretching techniques.
Note: Subluxation/Misalignment Versus Joint Dysfunction
The terms subluxation and misalignment are commonly used in chiropractic and osteopathic practices. Although these two terms are often used to denote joint dysfunction, they are not actually synonymous with joint dysfunction. Subluxation and misalignment, as well as saying that a bone is out of place refer to the static structural/postural alignment of a vertebra. If in neutral anatomic position, a vertebra is slightly rotated, laterally flexed, flexed, or extended, then it is said to be subluxated or misaligned. Joint dysfunction, on the other hand, refers to the functional motion of a vertebra at its spinal joints.
However, there often is a relationship between the static alignment of a vertebra and its functional motion. A vertebra that is misaligned is often misaligned because of asymmetry of tight musculature and/or adhesions. The same tight musculature and adhesions may certainly affect the motion of the vertebra, causing a hypomobile joint dysfunction. This relationship is not always present, however. A helpful analogy is that of a door that naturally sits slightly ajar. If you look at its static position, you would say that it is misaligned because it is ajar. However, to determine whether the door functions correctly, you would need to see if it can move through its full range of motion, opening and closing all the way. If it can do that, then it is functioning fine, even if it is “misaligned.” When there is a discrepancy between structure and function, proper functioning is usually more important.
Description of Joint Dysfunction
Joint dysfunction means that the function of a joint is unhealthy. Given that joint function is to allow movement, two forms of joint dysfunction exist. A hypomobile joint is restricted in motion and moves too little; a hypermobile joint has excessive motion and moves too much.
Although both hypermobilities and hypomobilities can occur in the lumbar spine and pelvis, the more common presenting complaint, and the one that manual therapists are better able to treat, is hypomobility. Because a lumbar spinal joint can move in multiple directions, it can be hypomobile in one or more of its six cardinal ranges of motion: flexion, extension, right and left lateral flexion, and right and left rotation. For example, it is possible for a lumbar spinal joint to move perfectly well into right lateral flexion (as well as other ranges of motion) but not move well into left lateral flexion. For this reason, to accurately assess a joint hypomobility, the specific range of motion that is restricted should be determined.
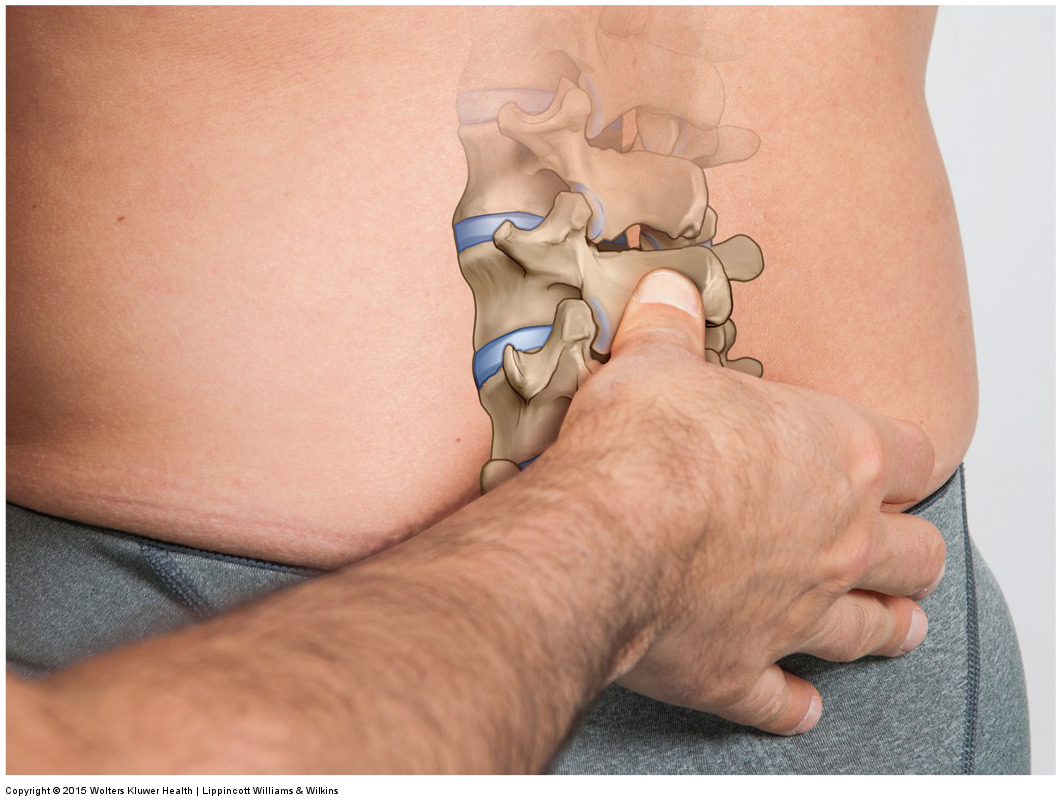
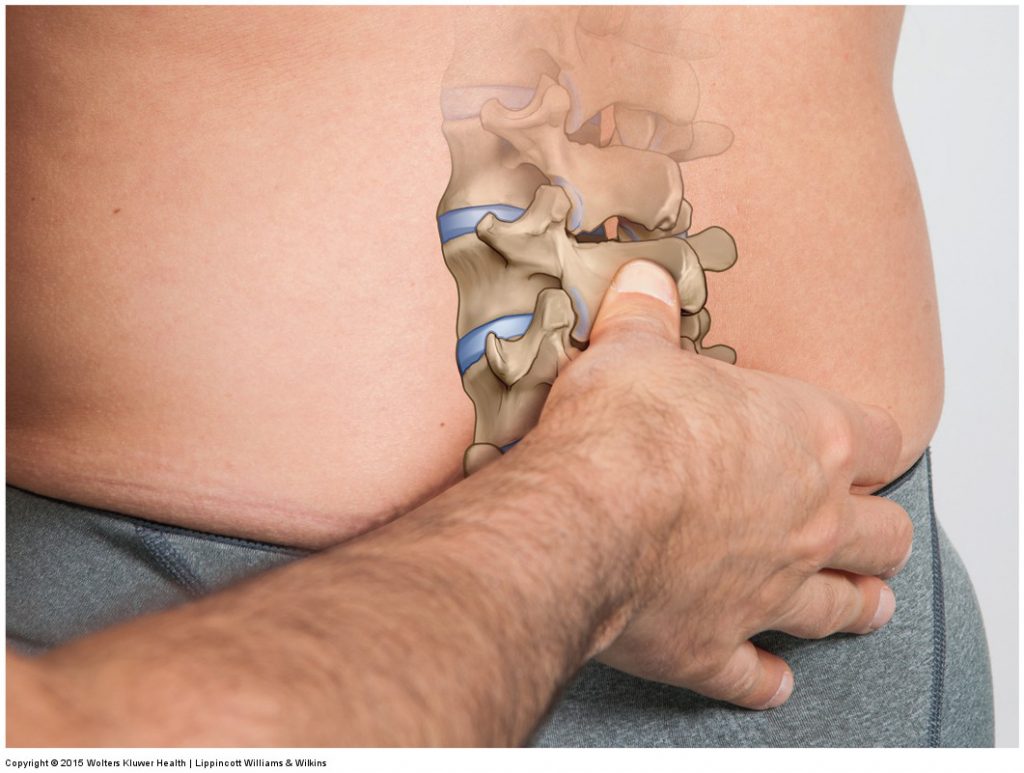
However, assessing the overall gross range of motion of a specific motion of the low back (such as right lateral flexion) does not necessarily indicate the range of motion of specific segmental joint levels of the low back. In other words, a client may have a full 45-degree range of motion into right lateral flexion of the lumbar spine as a whole; however, the client may be restricted and hypomobile within a specific portion of the lumbar spine, say at the L4-L5 segmental joint level. If the client is compensating with more motion at the adjacent L3-L4 joint level, then this hypermobile L3-L4 joint will mask the hypomobile L4-L5 joint level (Fig. 6).
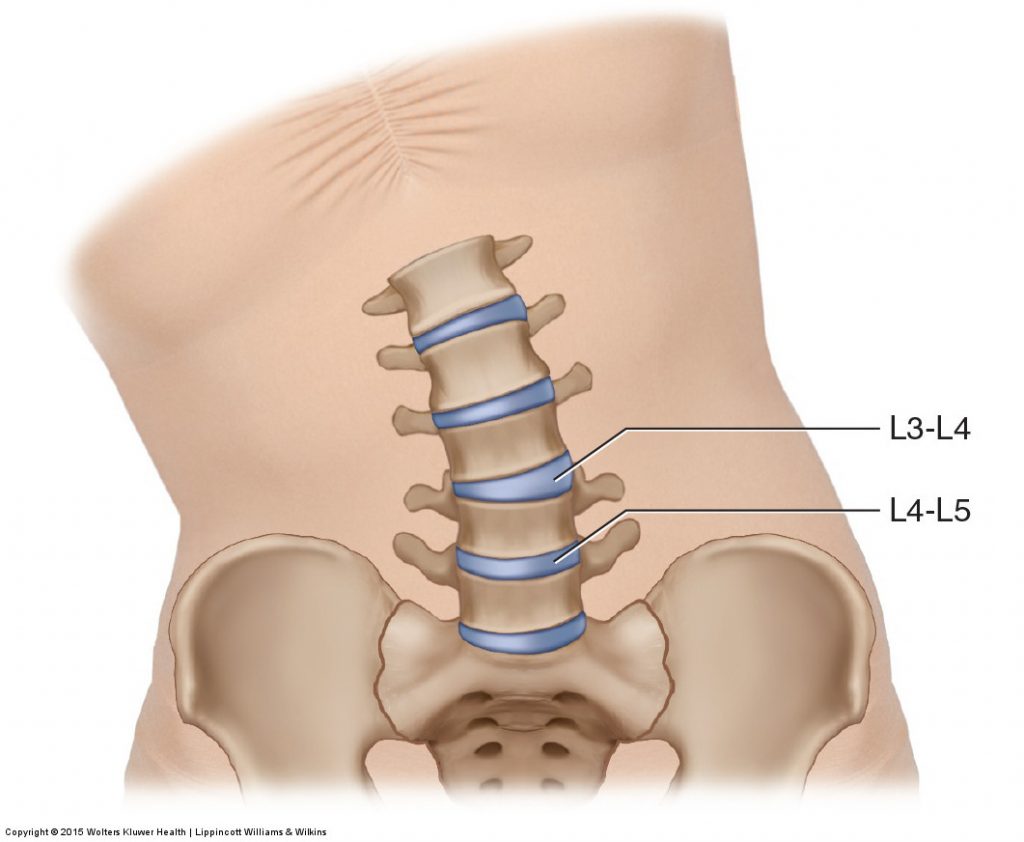
Figure 6. Joint hypomobility. A joint dysfunction hypomobility at one segmental level of the lumbar spine usually results in a compensatory joint dysfunction hypermobility at the adjacent level. Here, L4-L5 is hypomobile, and L3-L4 is a compensatory hypermobility. Permission Joseph E. Muscolino. Manual Therapy for the Low Back and Pelvis – A Clinical Orthopedic Approach. 2015.
Mechanism and Causes of Joint Dysfunction
There are usually two major mechanisms that can cause a hypomobile joint. One is tight (hypertonic) muscles that cross the joint; this is especially true of smaller, deeper intrinsic muscles of the joint, such as rotatores, interspinales, and intertransversarii of the low back. The other is taut soft tissues resulting from the buildup of fibrous adhesions; this is especially important if the adhesions build up in the joint capsules and ligaments of the joint because they directly and intimately limit the motion of the joint.
There are also two major mechanisms that cause a hypermobile joint. Certainly, an overstretching injury of the joint’s soft tissues, especially the joint capsules and ligaments, will result in an unstable hypermobile joint. Another common mechanism that creates a hypermobile joint is excessive joint movement in compensation for an adjacent hypomobility. This is especially true in the spine, where multiple joints are located next to each other.
The example used in the preceding section demonstrates why it can be important to detect early a segmental hypomobility. If L4-L5 is hypomobile and L3-L4 compensates by becoming hypermobile, in time, L3-L4 level will likely be overused and become fatigued and painful. This will lead to the pain-spasm-pain cycle, which in turn will result in a tightening of the smaller intrinsic muscles around the L3-L4 joint, causing it to become hypomobile as well. As a result, demand will be placed on the next segmental level, L2-L3, to become further hypermobile to compensate for the two hypomobile segments below it. Naturally, in time, this level may be similarly overused and then become hypomobile itself. Segmental joint dysfunction hypomobilities tend to have a domino effect, spreading through the spine until sufficient hypermobile compensation is not possible and the overall gross range of motion of the spine is decreased. However, this point is often reached late in the disease process. If not detected early, delayed treatment allows tight musculature to become chronic and more fascial adhesions to form. For this reason, it is important to locate and identify segmental joint hypomobilities early when only one, or perhaps two, are present. The assessment technique for segmental joint hypomobility is called motion palpation or joint play assessment. Treatment is then aimed at introducing motion into these restricted joints.
It should be emphasized that joint dysfunction is not necessarily a problem of the entire low back and/or pelvis. Rather, it is more focused on a specific segmental joint level of the region. When joint dysfunction of a segmental joint level occurs, it is often the result of a tightening of the smaller, deeper, intrinsic postural muscles that cross just that joint or perhaps a couple of joints in that area. Examples are the rotatores, multifidus, intertransversarii, or interspinales. Similarly, taut fascial tissues, likely the result of fascial adhesions, are not necessarily present in every area of the low back. Instead, they may be present in the joint capsules and ligaments of a specific joint level or a couple of joint levels. The same process that a manual therapist often sees on a larger level is simply being played out on a smaller, more focused level.
Note: Joint Dysfunction
Every technique presented in this book can be used to address hypomobile joint dysfunction. Massage and stretching can be used to loosen tight muscles associated with hypomobility as well as to stretch the taut soft tissues associated with it. However, the best technique to target the specific segmental hypomobilities is joint mobilization. Hydrotherapies can also be beneficial for softening and loosening these tight/taut soft tissues. Hypermobile joint dysfunction is more problematic to treat.
Note: Other Causes of Joint Hypomobility
In addition to tight musculature and fascial adhesions, two other mechanisms exist that can cause joint hypomobility. One is bone spur formation at the joint margins; this is part of the DJD process (DJD is covered in more detail later in this chapter). If a bone spur becomes large enough, it can block and limit joint motion at that segmental level. The other mechanism is the presence of a meniscoid body within the joint space. A meniscoid body is a fibrous, fatty, soft tissue that is usually present at the periphery of a joint space. The meniscoid body functions to increase the congruity of the joint by helping the two joint surfaces better fit together. However, if it displaces and moves toward the center of the joint, it can jam between the two bones and cause a blockage and restriction of motion (see accompanying figure).
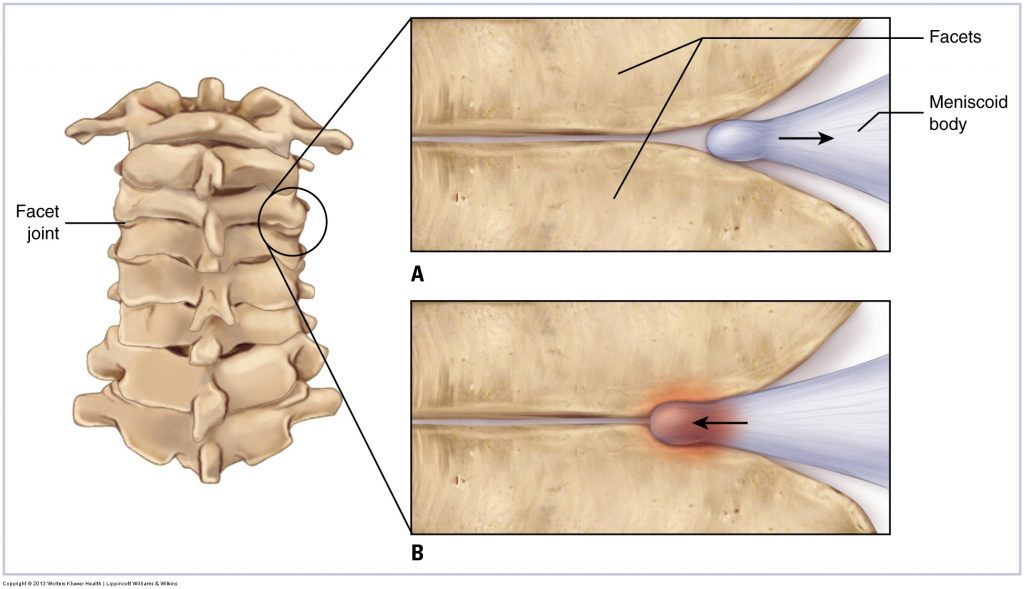
(A) A meniscoid body’s normal and healthy relationship to the facet joint. (B) A meniscoid body jammed between the two facets of the joint. Permission Joseph E. Muscolino. Manual Therapy for the Low Back and Pelvis – A Clinical Orthopedic Approach. 2015.
(Note: Click here for a blog post article on joint dysfunction of the cervical spine.)
This blog post article is the third in a series of twelve articles on musculoskeletal conditions of the low back (lumbar spine) and pelvis.
The articles in this series are:
- Hypertonic / tight muscles
- Myofascial trigger points
- Joint dysfunction
- Sprains and strains
- Sacroiliac joint injury
- Pathologic disc conditions and sciatica
- Piriformis syndrome
- Degenerative joint disease (DJD)
- Scoliosis
- Lower crossed syndrome
- Facet syndrome
- Spondylolisthesis