Osteoarthritis (OA), also known as degenerative joint disease (DJD) is a disease in which the joints deteriorate. DJD is a normal response to the physical forces that are placed on the joints as we age. However, if the degree of progression is either more than is typical for the client’s age or impairs function, it is considered a pathologic disease process. When this condition occurs in the spine, it is also called spondylosis. Most older middle-aged and elderly clients who state that they have “arthritis” have OA/DJD.
Note: The Terms Degenerative Joint Disease and Osteoarthritis
Arthritis literally means “joint inflammation” (“arthr” means joint; “itis” means inflammation). The term degenerative joint disease is gradually replacing the term osteoarthritis because inflammation is rarely involved, making the suffix “itis” inappropriate. Inflammation is usually present only when the condition has progressed and is more severe.
Description of Degenerative Joint Disease
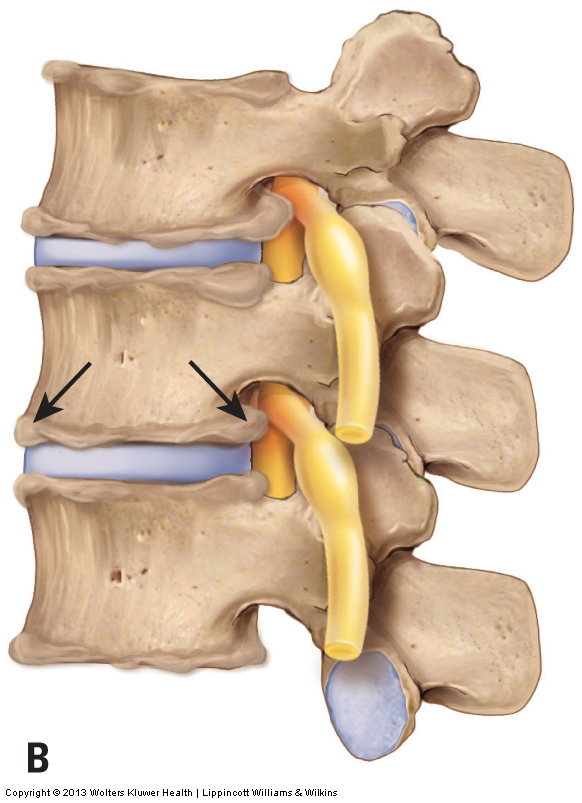
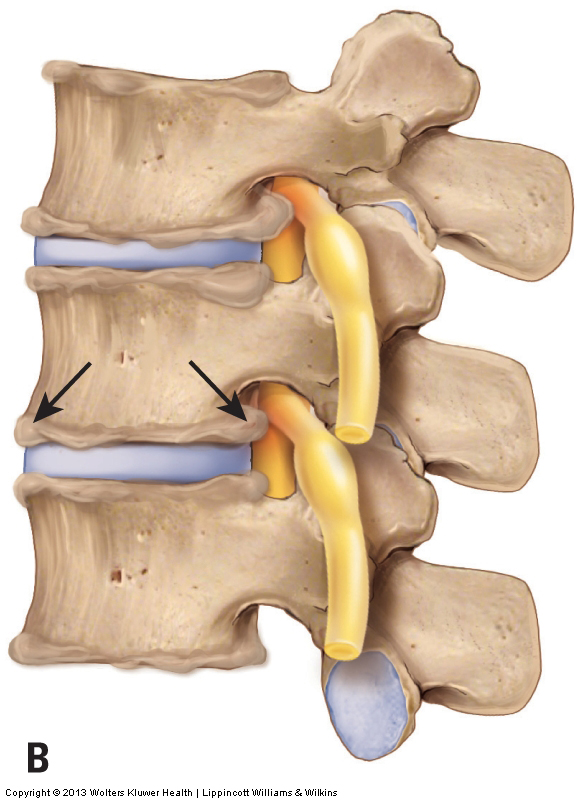
The beginning stage of DJD involves breakdown of the articular cartilage that covers the joint surfaces of the two bones of the joint. As the condition progresses, calcium is deposited within the bone that underlies the articular cartilage (subchondral bone). In later stage of DJD, calcium deposition begins to occur on the outer surfaces of the bones of the joints, and bone spurs (also known as osteophytes or lipping and spurring) protrude at the joint margins (Fig. 17). DJD can affect both the disc and facet joints of the spine. These bone spurs are easily seen on radiography (X-Ray), making radiographic analysis the best and easiest means to assess DJD.
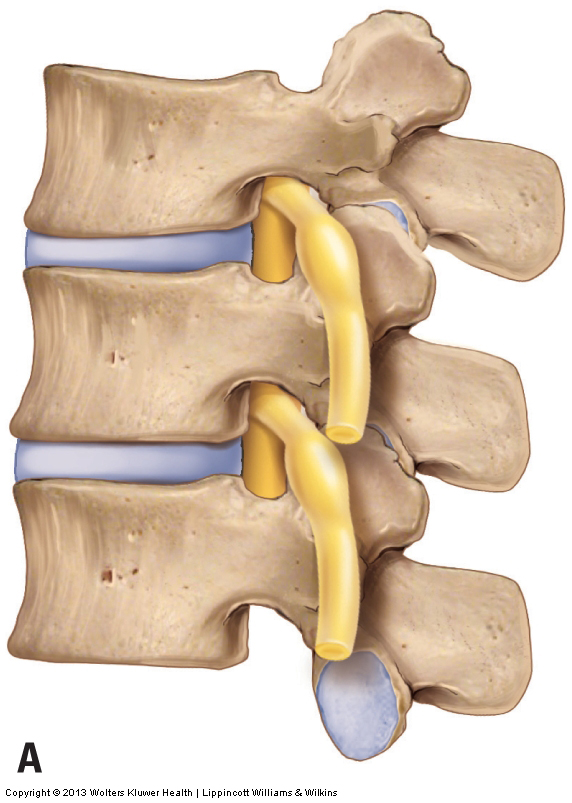
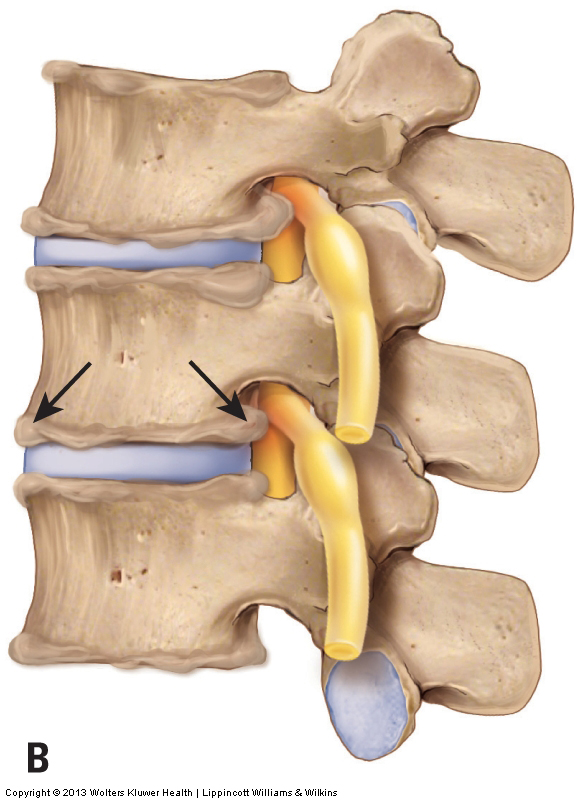
Figure 17. Osteoarthritis (OA), also known as Degenerative Joint Disease (DJD). A, Healthy spine. B, OA/DJD bone spurs along the joint margins.
Because DJD occurs as a result of accumulated physical stresses, radiographs (x-rays) of most middle-aged people will reveal at least some cervical spinal DJD. Most of the time, the presence of DJD is an incidental finding and the condition causes no symptoms. However, if the condition progresses to the point of functional impairment, a decrease of motion can occur at the joint where the DJD is present. This is a result of the presence of bone spurs that block full range of motion of the affected joint. Furthermore, if the calcium deposition creates bone spurs that are large enough to encroach on the spinal nerve in the intervertebral foramen or on the spinal cord within the spinal canal, the calcium deposition can cause compression of nervous tissue, resulting in referral (radiculopathy) into the upper extremities. When the calcium deposits of DJD cause compression of a spinal nerve or the spinal cord, DJD is similar in mechanism to a bulging or ruptured disc in that it is a space-occupying lesion that compresses nerve tissue.
Note: Is Osteoarthritis the Cause of the Client’s Pain?
Osteoarthritis (Degenerative Joint Disease / DJD) must be fairly marked in its progression to actually compress spinal nerves or the spinal cord and cause symptoms. However, physicians often wrongly blame DJD for a client’s pain when the pain is actually caused by tight muscles and other taut or irritated periarticular (extra-articular/extrinsic) soft tissues located around the joint. Tight muscles are probably the most common aggravated periarticular soft tissue. When the physician orders and views radiographs of the client’s neck, if any DJD is present, as is usually the case in most middle-aged and older adults, it may be blamed for the client’s pain. But the muscles and other soft tissues are not visible on radiographs, and these tissues often are the true culprit. When this is the case, the manual therapist can provide an important service by relaxing, softening, and loosening the muscles and other soft (fascial) tissues of the neck. Further, because tight muscles and other soft tissues can add to the physical stress on joints, improving the health of the soft tissues can also decrease the progression of the client’s DJD and possibly even help to keep it from causing nerve compression.
Mechanism and Causes of Degenerative Joint Disease
The mechanism of DJD is a simple wear and tear response of the cartilage and bony surfaces of a joint resulting from the physical stress that is placed on the bones at the joint. If the degree of physical stress is more than the joint can absorb, the articular cartilage begins to degrade, and in so doing, more stress is transmitted to the subchondral bone. Excessive stress on the subchondral bone then causes calcium to be deposited along the margins of the bones of the joint, a physical process known as Wolff’s law. Wolff’s law states that calcium is deposited in response to the physical stress that is placed on a bone. This process is meant to strengthen bone by increasing its calcium mass; however, if the stresses placed on the bone are excessive, excessive calcium deposition occurs, resulting in bone spurs, as described previously. Movement and weight bearing are everyday microtrauma stresses that affect joints. Tight musculature, especially chronically tight postural muscles, can also be viewed as repeated microtrauma that adds compression forces to the joints that the tight muscles cross. Certainly, more powerful macrotraumas, such as falls and whiplash accidents, can also greatly contribute to the progression of DJD.
Other factors may also contribute. Decreased strength/facilitation of stabilization musculature around the joint may allow for unhealthy arthrokinematics (joint movement) that may contribute to the development of osteoarthritis. There may likely be a genetic component as well. And some sources believe that inflammatory conditions also increase the development of osteoarthritis.
Note: Treatment Considerations in Brief for Osteoarthritis (Degenerative Joint Disease/DJD)
Massage can be extremely beneficial in helping to decrease the muscular spasms that often coexist with and increase the physical stresses that foster DJD. Stretching is also helpful for the taut soft tissues that likely exist. However, if the DJD is advanced to the point that it is causing neural compression, then the client should not be laterally flexed to the side of a bone spur or placed in any position that causes or increases referral of symptoms into the upper extremity. If neural compression and/or nerve irritation is present, icing may help to decrease some of the accompanying inflammation.
Of course, with any manual therapy treatment to the neck, there are always precautions and contraindications to consider given the number of sensitive structures present.
Note: All figures courtesy Joseph E. Muscolino. Originally published in Advanced Treatment Techniques for the Manual Therapist: Neck. 2013.
(Click here for the blog post article: 10 Health Benefits and Uses for Tumeric Curcumin Supplements.)
Note: This blog post article is the sixth in a series of 10 posts on
Common Musculoskeletal* Conditions of the Neck
The 10 Blog Posts in this Series are:
- Fascial Adhesions (and an introduction to musculoskeletal conditions of the neck)
- Hypertonic (tight) musculature
- Joint dysfunction
- Sprains and strains
- Pathologic disc conditions
- Osteoarthritis (OA)
- Thoracic outlet syndrome (TOS)
- Forward head posture
- Tension headaches
- Greater occipital neuralgia
(*perhaps a better term is “neuro-myo-fascio-skeletal”)