Note: This blog post article is the first in a series of six posts on the
Anatomy / Structure of the Cervical Spine for Manual and Movement Therapists.
The Six Blog Posts in this Series are:
- Introduction to the Cervical Spine
- Cervical Spinal Joints
- Motions of the Cervical Spine
- Musculature of the Cervical Spine
- Ligaments of the Cervical Spine
- Precautions When Working the Neck
The neck is defined by the cervical spine. The cervical spine is composed of seven vertebrae, named C1 to C7 from superior to inferior; C1 is also known as the atlas and C2 is also known as the axis (Fig. 1). (The occiput above the cervical spine is often described as C0.) From a lateral view, the healthy cervical spine can be seen to have a lordotic curve (lordosis), which is defined as being concave posteriorly and convex anteriorly. (The terms lordotic and lordosis are often used to denote an excessive and unhealthy lordotic curve. However, these terms are also used to refer to the healthy and normal curve of the neck and low back.) All cervical vertebrae except for the atlas have a spinous process that extends posteriorly and that can be palpated. Instead of a spinous process, the atlas has a small tubercle at the back of its arch that is called the posterior tubercle. The posterior tubercle of the atlas is usually not easily palpable.
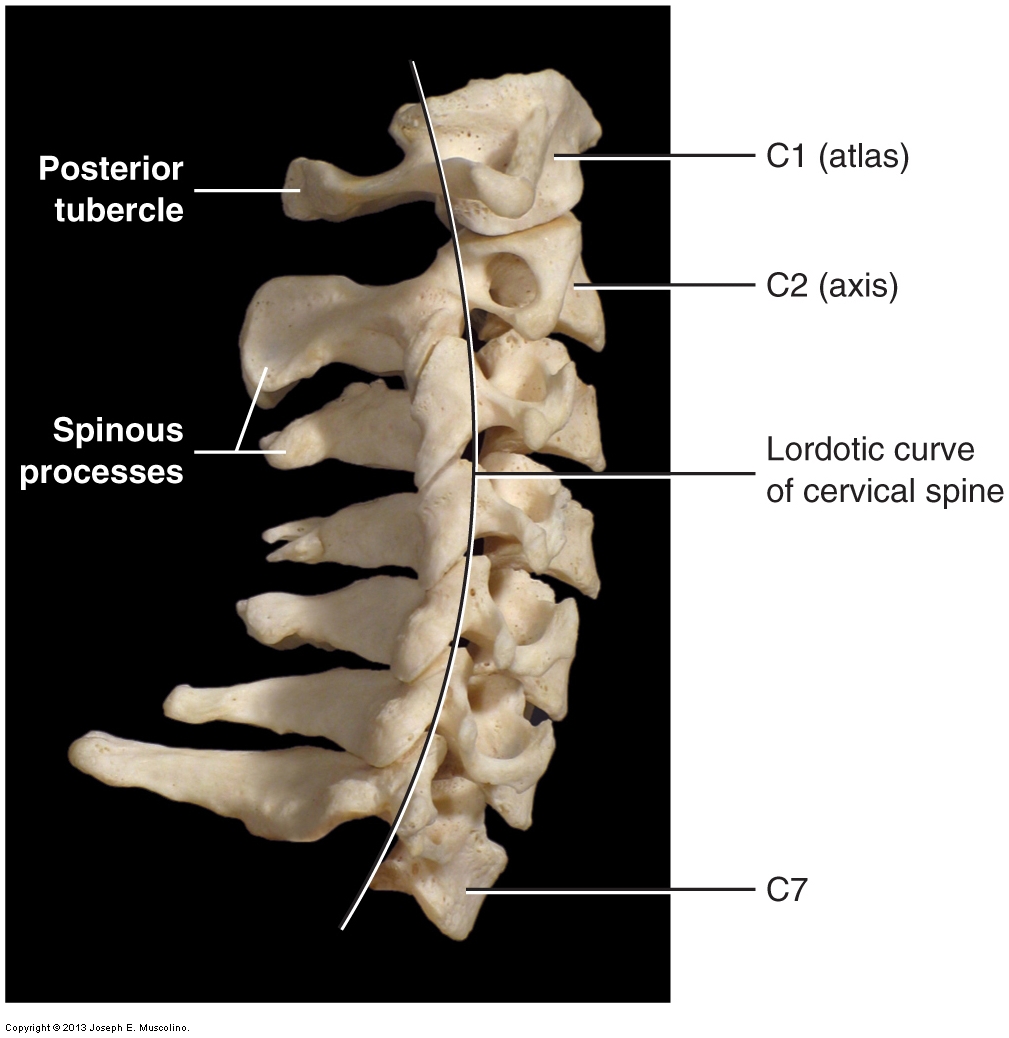
Figure 1. Right lateral view of the cervical spine. The cervical spine’s curve is described as lordotic, with its concavity facing posteriorly and its convexity facing anteriorly. The seven vertebrae of the cervical spine are numbered C1-C7 from superior to inferior. C1 is also known as the atlas; C2 is also known as the axis. (Courtesy of Joseph E. Muscolino. Photography by David Eliot.)
Of all the cervical spinous processes, those of C2 and C7 are most easily palpable. Generally, the spinous process of C2 is clearly palpable in the upper neck and the spinous process of C7 is clearly palpable in the lower neck. How easy or difficult it is to palpate the spinous processes of C3-C6 depends largely on the degree of the client’s lordotic curve. Because the cervical curve is lordotic, the spinous processes are recessed and not as superficial for palpation. However, some clients’ cervical curves are decreased or even straight; a decreased or absent lordotic curve is termed hypolordotic, making palpation of all of the spinous processes quite easy. An important feature to note regarding the cervical spinous process is that it is bifid, meaning that instead of coming to one point, it splits to have two points at its end. The degree to which a cervical spinous process is bifid can vary (generally, C7’s spinous process is not bifid). The bifid shape of the spinous processes of the cervical spine is visible in Figure 2 (see also Fig. 3B). Knowing about this bifid shape is important in manual therapy work because sometimes the two points of the bifid spinous process are not symmetrical in shape or equal in size, making it possible to inaccurately assess the vertebra as being malpositioned in rotation.
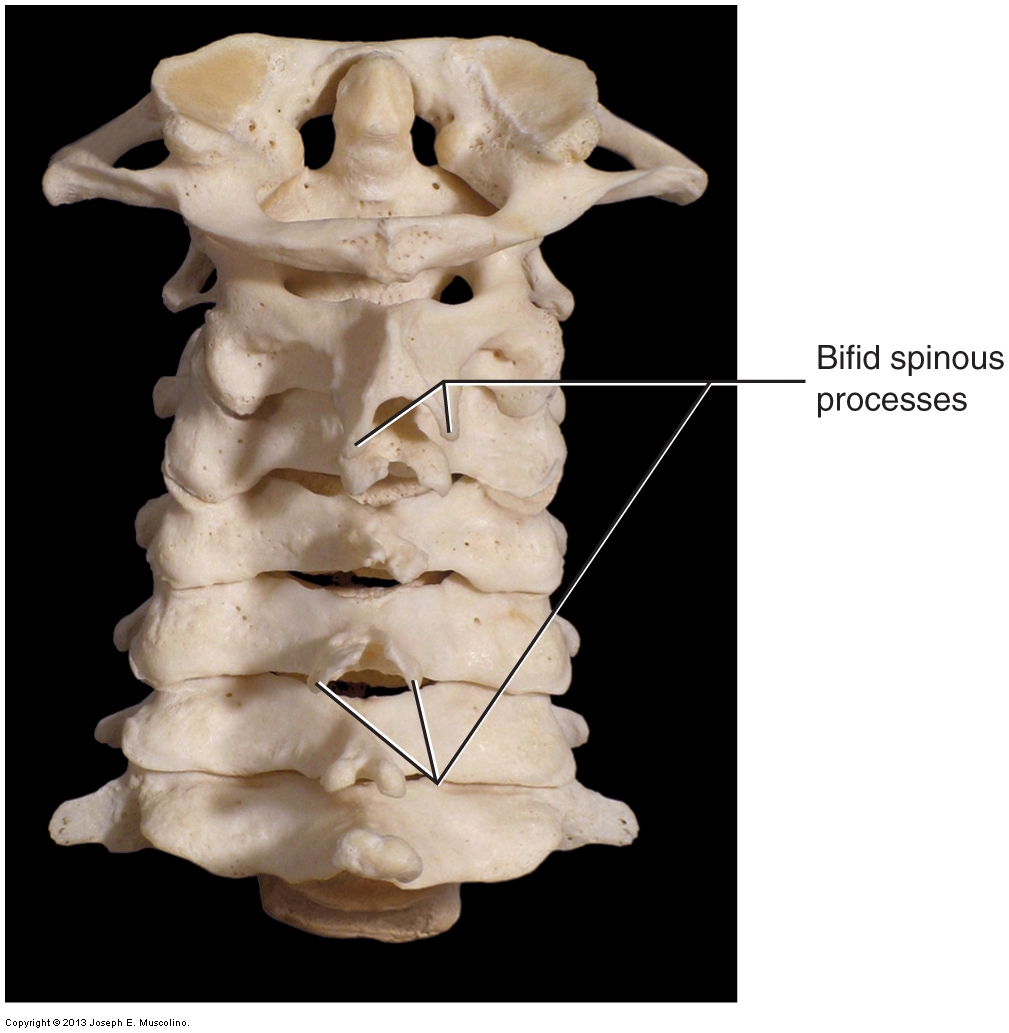
Figure 2. Posterior view of the cervical spine. Its bifid spinous processes are visible. (Courtesy of Joseph E. Muscolino. Photography by David Eliot.)
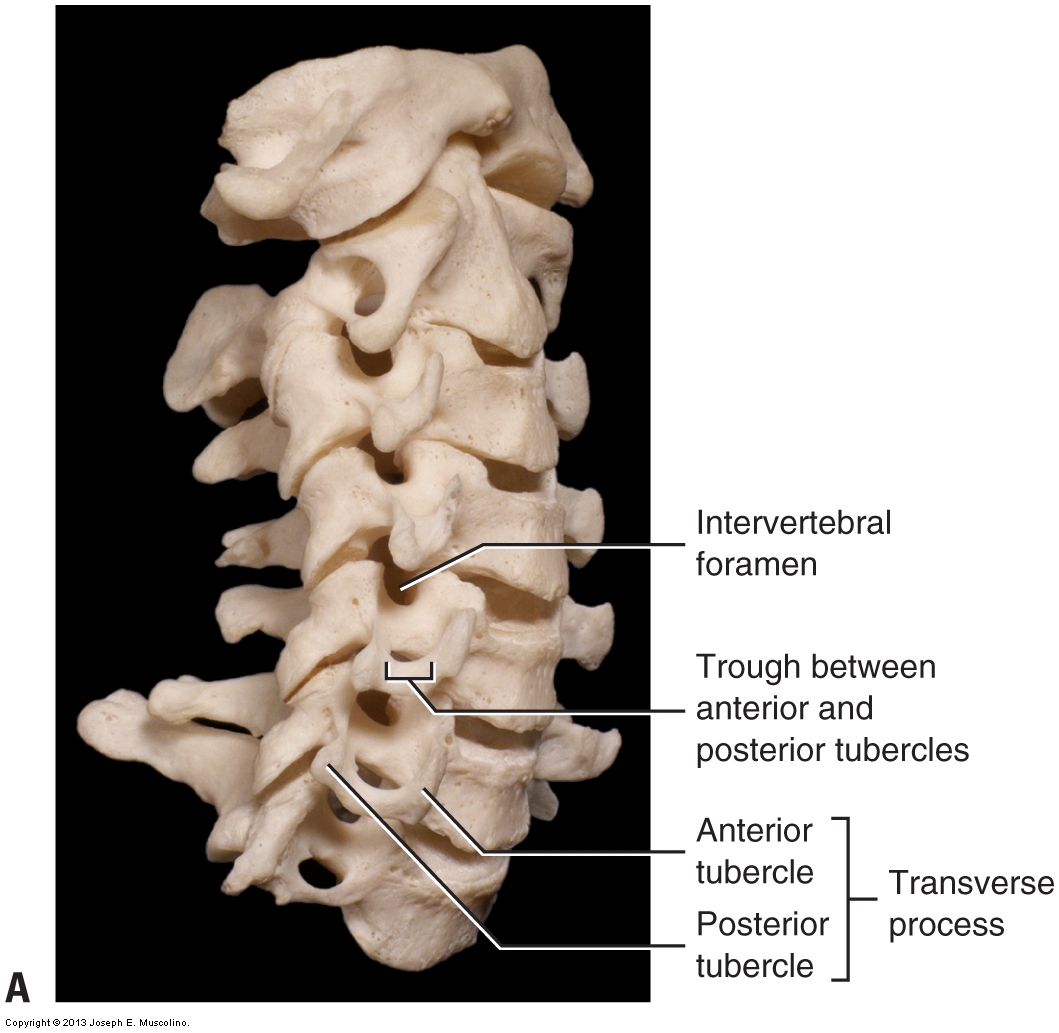
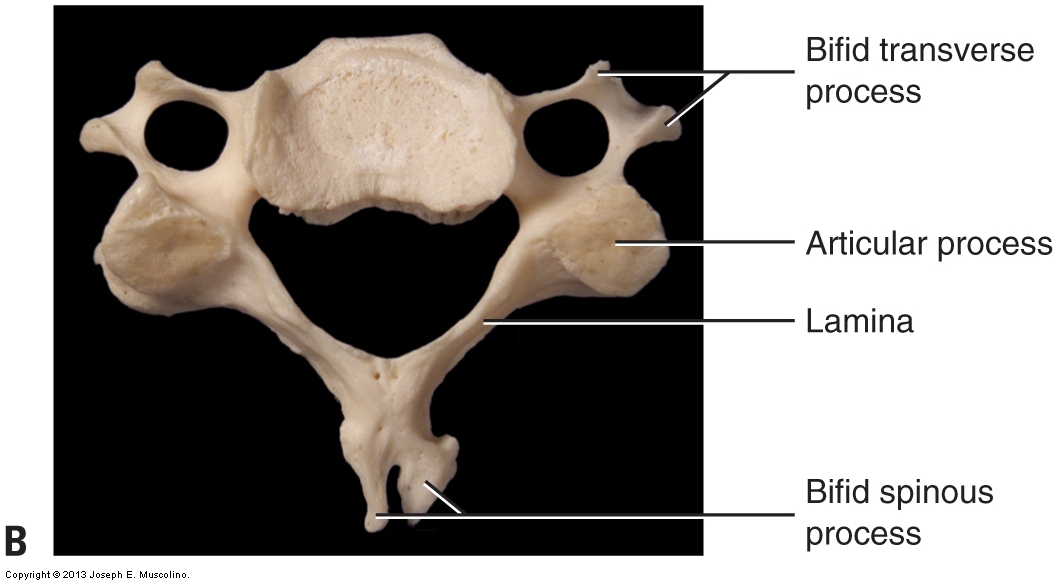
Figure 3. Bifid transverse processes of the cervical spine. The bifid transverse processes of the cervical spine split into an anterior tubercle and a posterior tubercle. (A) Right anterolateral oblique view. (B) Superior view of a typical cervical vertebra.(Courtesy of Joseph E. Muscolino. Photography by David Eliot.)
The transverse processes of the cervical spine extend laterally and are also bifid. Each transverse process splits to form a posterior tubercle and an anterior tubercle (Fig. 3). These tubercles tend to be sharply pointed, and it can be quite uncomfortable for the client to have them palpated. For this reason, palpation of the transverse process attachments of the neck muscles should be done gently, carefully, and slowly. As a rule, the transverse processes should not be used as a contact point for pressing on the cervical spine, such as when doing deep tissue massage, stretching the client’s neck, or performing joint mobilization (whether this is Grade IV “arthrofascial stretching” joint mobilization or Grade V “chiropractic” joint mobilization / joint manipulation). Caution should also be exercised when palpating in the region of the transverse processes, because the cervical spinal nerves that enter or exit the spinal cord through an intervertebral foramen travel in a trough/channel formed by the anterior and posterior tubercles of the transverse process. In addition to being uncomfortable for the client, imprudent or excessive pressure at the transverse processes could cause compression of the cervical spinal nerves.
Given the pointed shape of the cervical spinous and transverse processes, the best contact points on the client’s neck are across the lamina and the articular process at that vertebral level (Fig. 4A). The position of the lamina between the spinous process and articular process creates what is known as the laminar groove, which is located posterolaterally on the spine.
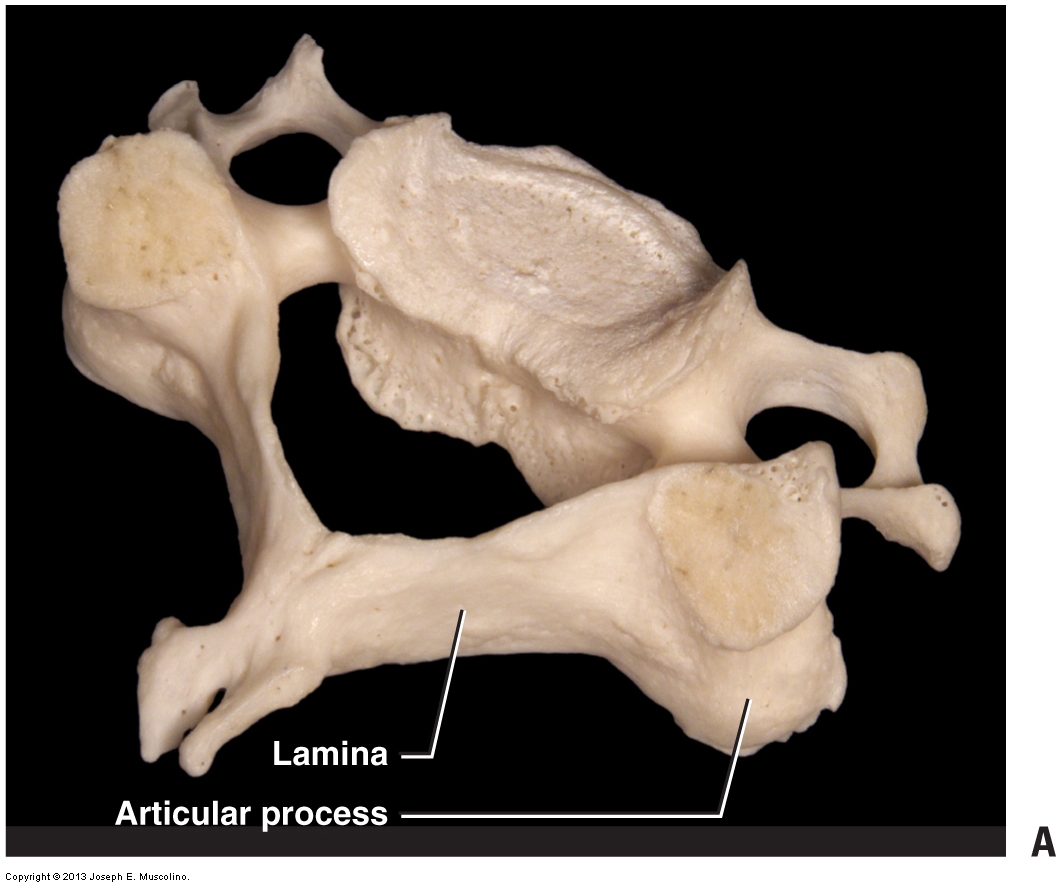
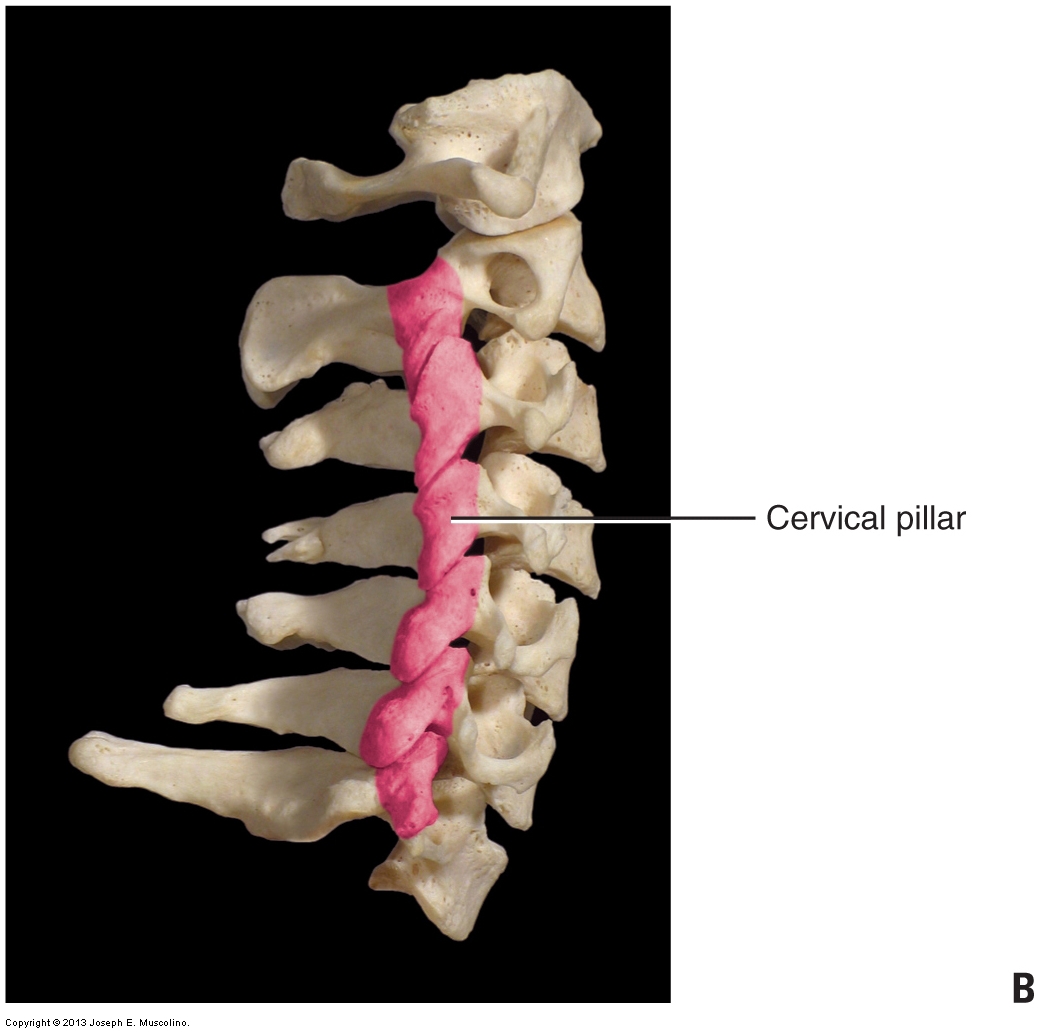
Figure 4. Laminar groove and articular pillar. (A) Right oblique (superior posterolateral) view of a typical cervical vertebra. The lamina/laminar groove and articular process of the vertebra are seen. (B) Stacking of the articular processes of the cervical spine creates the cervical pillar (articular pillar). (Courtesy of Joseph E. Muscolino. Photography by David Eliot.)
There are two reasons why it is important to be able to locate and palpate the laminar groove and/or articular process:
- The laminar groove is where the majority of the musculature of the spine is located. In particular, the semispinalis, multifidus, and rotatores of the transversospinalis group are located here, and the semispinalis capitis is the thickest muscle of the neck. Hence, when working the posterior musculature of the neck, much of the work needs to be done in the laminar groove.
- The laminar groove and articular process of a cervical vertebra provide a large flat surface that serves as an ideal contact surface when working on a client. The articular process in particular is ideal as a contact point when applying force onto the client’s spine for stretching and joint mobilization. With the stacked structure of the cervical vertebral column, the articular processes create the cervical pillar or articular pillar (Fig. 1-4B), a stable column of bone that is an ideal contact point for the therapist throughout the cervical spine.
All photos courtesy of Joseph E. Muscolino. Originally published in Kinesiology: The Skeletal System and Muscle Function, 3ed. 2017. Elsevier.


