Signs and symptoms of lower crossed syndrome:
The first and most obvious sign of (Vladimir Janda’s) lower crossed syndrome is the characteristic postural dysfunction of increased anterior pelvic tilt with hyperlordotic lumbar spine. Upon palpation, the following muscles will most likely be found to be tight: tensor fasciae latae (TFL), rectus femoris, iliacus, psoas major, pectineus, adductors longus and brevis, thoracolumbar paraspinals (erector spinae and transversospinalis) and quadratus lumborum. And the client/patient will feel restriction of the following motions: extension of the thigh at the hip joint and flexion of the low back (thoracolumbar spine) at the spinal joints.
Although pain is not necessarily a part of this condition, when this condition has existed for a long time, the client does often experience low back pain, both due to the tightness of the low back extensor musculature and the psoas major, and due to the increased compression upon the facet joints of the lumbar spine. This condition is called facet syndrome. If facet compression is symptomatic, the client’s pain pattern will increase with extension of the lumbar spine. Pain might also be experienced in the anterior (hip flexor) and medial (adductor) hip joint regions. If left unresolved for a long period of time, the development of upper crossed syndrome and all its sequelae are also likely to occur as a consequence of lower crossed syndrome.
Assessment/Diagnosis of lower crossed syndrome:
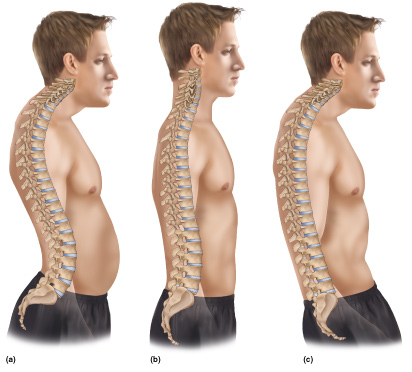
Visual observation assessment of the posture of the lumbosacral region of the body for lower crossed syndrome. Permission: Joseph E. Muscolino. Art work by Giovanni Rimasti.
Assessment/diagnosis of lower crossed syndrome follows from the signs and symptoms of this condition. The most important assessment tool is static postural assessment, which will reveal the characteristic excessive anterior pelvis tilt and hyperlordotic lumbar spine. Upon palpatory examination, tightness and the likely presence of myofascial trigger points will be found in the overly facilitated muscles listed above. Due to the gluteus maximus being weak/inhibited, it is also likely that the hamstrings will be tight/facilitated.
Verbal history might likely reveal habitual seated posture and postures of leaning forward, as well as a lack of exercise of the core anterior abdominal wall and posterior gluteal musculature.
Lower crossed syndrome is a dysfunctional postural condition of the musculoskeletal system, so no further medical diagnosis/assessment is needed. However, if X-Rays are done, not only will the altered posture of the lumbosacral spine be easily visualized on the lateral view (and the sacral base angle can be measured – see other blog article on this condition), but the posterior wedging of the lumbar vertebral bodies might also be visible in clients who have had this condition for many years. Note: It is best to have these X-Rays done with the client standing so that the effects of gravity can be seen.
Differential assessment of lower crossed syndrome:
Assessment of lower crossed syndrome is straightforward and simple; therefore no differential assessment is necessary. If the client/patient has the characteristic lower crossed posture, lower crossed syndrome can be assessed with confidence. However, this does not mean that the client does not have the presence of additional conditions that should be assessed. The presence of any musculoskeletal condition, especially such a pervasive postural dysfunctional pattern like lower crossed syndrome that affects the entire pelvis and lower spine often necessitates compensation patterns that can then create other conditions. Look especially for facet syndrome and upper crossed syndrome.


