Self-care for the client/patient with hamstring strain:
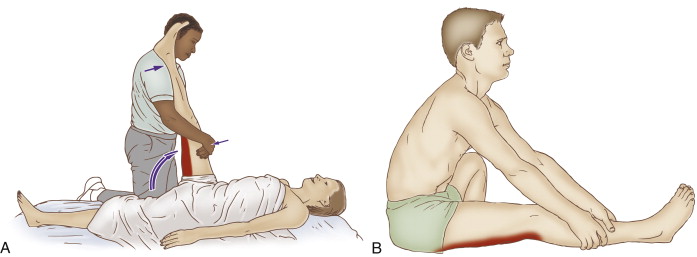
Self-care (and therapist assisted) stretch for the hamstring group. Permission: Joseph E. Muscolino. The Muscle and Bone Palpation Manual, with Trigger Points, Referral Patterns, and Stretching, 2ed. (2016) Elsevier.
Self-care for the client/patient with a hamstring strain during the acute stage is RICE: rest, ice, compression, and elevation. Of these, rest and ice are most important. Icing should be applied until the area is numb and then removed. Flexible gel ice packs are best, especially when the pack needs to contour to the client’s/patient’s body. For client comfort, a paper towel or thin cloth towel should be placed between the pack and their skin. The client/patient can also stretch and if possible strengthen the opposite-side hamstrings for the neural cross-over effect.
During later stages of treatment of a client with a hamstring strain, moist heat and stretching are extremely important so that the area does not heal with excessively tight muscle tone, myofascial trigger points, and myofascial adhesions. Instruct the client/patient on how to stretch into thigh flexion with the knee joint extended. One method is for the client/patient to sit on the floor with their knee joint extended and then rock forward the pelvis, in other words anteriorly tilt the pelvis at the hip joint. Make sure that the client/patient does not place the other lower extremity in an unhealthy position that would torque the knee joint. An alternative position is to lie down and use a rope or belt looped around the foot to passively bring the thigh into flexion. Be sure to advise the client/patient to avoid hyperextending their knee joint. This can be done in the seated position by placing a small rolled up towel under the knee.
During the chronic stage of hamstring strain, activity can be gradually reintroduced, as long as it is done incrementally in baby steps. It is also extremely important for the client to warm up extremely well before working out. The best form of warm up involves active/dynamic stretching so that local circulation of fluids (blood, lymph, and synovial joint fluid) is increased, muscles are stretched and contracted, and neural patterns for movement are facilitated. After the physical activity is completed, then the client can perform static stretching.
Medical approach to hamstring strain:
The typical medical approach to hamstring strain is RICE. Anti-inflammatory medication is often prescribed; this might be non-steroidal (NSAID) or steroidal (cortisone/prednisone). If the strain is severe, X-Rays or an MRI will usually be ordered to rule out full rupture from the ischial tuberosity of one or all of the hamstrings. If a rupture is found, surgery is performed. After surgery, the client/patient must wear a brace for approximately 6-8 weeks to immobilize the hip joint and allow the tissue to heal.
Manual therapy case study for hamstring strain:
Alex is a 26-year-old fitness trainer who was rock climbing when he forcefully pushed off with his left lower extremity and felt a sudden sharp pain in the back of his thigh near his ischial tuberosity. The pain continued so he stopped climbing and went home. Upon awakening the next morning, his left thigh felt stiff and the pain was still present so he went to see a clinical orthopedic massage therapist who had worked on him in the past.
Upon examination, the therapist observed swelling and bruising approximately two inches distal to the ischial tuberosity. The area was hot to touch and pain was elicited with even mild pressure. The therapist palpated what felt like a small indentation along the course of the biceps femoris near the proximal musculotendinous junction. Any attempt by Alex to actively extend his thigh brought on immediate pain, as did passive flexion with his knee joint extended. The therapist assessed Alex as having a hamstring strain. Because of the acuteness of the injury, the therapist iced the region and performed a few minutes of extremely gentle distal-to-proximal effleurage strokes to the left hamstring musculature. Because Alex was limping, the therapist decided to spend the remainder of the time working his low back and the rest of his lower extremities. The therapist also stretched the right hamstring group with the purpose of creating some neural cross-over inhibition of the left side hamstring musculature.
The therapist gave Alex self-care advice regarding icing and continuing to stretch his right-side hamstrings, and cautioned him to refrain from any physical activity while the strain was healing. The therapist also recommended a treatment frequency of once per week for the first four weeks while the injury was acute, and then to increase the frequency of care to twice per week once the acute inflammatory stage had passed.
The therapist continued with the same treatment approach, but very gradually increased the depth of pressure and the amount of time spent working on the left hamstrings as Alex’s hamstring musculature gradually healed. By the fourth week, because the acute strain was well healed, the therapist increased the frequency of care to twice per week and the goal of therapy transitioned to working with moist heat, moderate to deep pressure soft tissue manipulation (massage), and stretching to loosen the general tightness and myofascial trigger points that had developed, and to prevent excessive scar tissue adhesions from developing. Alex was also able to carefully begin working out again to regain strength in his hamstrings. At the end of eight weeks, Alex’s condition was healed and his hamstring flexibility was back to pre-injury status.


